Transplanting patients’ own lung cells offers hope of ‘cure’ for COPD
Milan, Italy: For the first time, researchers have shown it is possible to repair damaged lung tissue in patients with chronic obstructive pulmonary disease (COPD) using the patients’ own lung cells.
The European Respiratory Society International Congress in Milan, Italy [1], heard that 17 patients who took part in a phase I clinical trial were able to breath better, walk further and had better quality of life after receiving the experimental treatment.
COPD kills approximately three million people worldwide every year. It is a severe respiratory disease that involves progressive damage to lung tissue. The affected tissue cannot be repaired with current treatments, only alleviated with medicines that widen the airways to improve airflow, known as bronchodilators.
To find new treatments for COPD, researchers have been investigating stem cells, which are capable of differentiating into any cell in the body, and progenitor cells, which are descendants of stem cells and can only differentiate into the cells that belong to the same tissue or organ and are normally used by the body to repair and replace damaged tissue. However, to date, the results have been conflicting, particularly for stem cells.
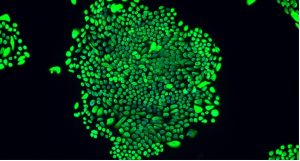
Professor Wei Zuo, of the School of Medicine, Tongji University, Shanghai, China, and chief scientist at Regend Therapeutics Ltd in China, and his colleagues have been investigating whether a type of cell called P63+ lung progenitor cells might be able to regenerate lung tissue damaged by COPD.
“Stem cell and progenitor cell-based regenerative medicine may be the biggest, if not the only, hope to cure COPD,” he told the congress. “P63+ progenitor cells are known for their ability to regenerate the tissues of the airways, and previously we and other scientists have shown in animal experiments that they can repair the damaged epithelial tissue in the alveoli – the tiny air sacs in the lungs that play a crucial role in the exchange of gases between air breathed in and the blood supply to the lungs.”
In this first phase I clinical trial, the researchers set out to investigate the efficacy and safety of taking P63+ progenitor cells from the lungs of 20 COPD patients, using them to grow millions more in the laboratory, before transplanting them back into the patients’ lungs.
“In our trial, 35% of the patients had severe COPD and 53% had extremely severe COPD. Usually, many patients with such severe COPD will die quite quickly if their disease progresses. We used a tiny catheter that contains a brush to collect the progenitor cells from the patients’ own airways. We cloned the cells to create up to a thousand million more, and then we transplanted them back into the patients’ lungs via bronchoscopy in order to repair the damaged lung tissue.”
Of the 20 patients, 17 were treated in this way and three were not and constituted the control group. They were assessed within 24 weeks of treatment to evaluate how well they tolerated the treatment and its effectiveness.
The cell treatment was well tolerated by all patients. After 12 weeks, the median (average) diffusing capacity of the lungs (DLCO), which tests how well air is exchanged between the lungs and the bloodstream, increased from 30% before treatment to 39.7%, and then increased further to 40.3% at 24 weeks in the treated patients. The median distance covered in a six-minute walk distance test (6MWD) increased from 410 metres before treatment to 447 metres at 24 weeks. The median score in a quality-of-life test (St George’s Respiratory Questionnaire or SGRQ) reduced by seven points, indicating an improvement. In two patients with mild emphysema, a type of lung damage that is normally permanent and progressive, the treatment repaired the lung damage.
Prof. Zuo said: “We found that P63+ progenitor cell transplantation, not only improved the lung function of patients with COPD, but also relieved their symptoms, such as shortness of breath, loss of exercise ability and persistent coughing. This means that the patients could live a better life, and usually with longer life expectancy.
“If emphysema progresses, it increases the risk of death. In this trial, we found that P63+ progenitor cell transplantation could repair mild emphysema, making the lung damage disappear. However, we cannot repair severe emphysema yet.”
The researchers are planning a phase II trial of the treatment, which will evaluate its efficacy in a larger group of patients. The trial has been approved by China’s National Medical Products Administration (NMPA), the Chinese equivalent of the US Food and Drugs Administration (FDA). This means that the treatment is not generally available to COPD patients and their doctors yet.
“However, with more doctors and patients participating in our clinical trial, we may develop the treatment more quickly so that it can benefit patients sooner,” said Prof. Zuo. “A similar therapeutic strategy is also being tested in patients with lethal lung fibrotic diseases, including idiopathic pulmonary fibrosis. We are going to test the treatment’s efficacy in larger groups of people with more lung diseases. We hope to develop the treatment for clinical use within about two to three years.”
Professor Omar Usmani, of Imperial College London (UK), is Head of the European Respiratory Society group on airways disease, asthma, COPD and chronic cough. He commented: “The results from this phase I clinical trial are encouraging. COPD is in desperate need of new and more effective treatments, so if these results can be confirmed in subsequent clinical trials it will be very exciting. It is also very encouraging that two patients with emphysema responded so well. A limitation of this study is that the uptake of the progenitor cells when they were transplanted back into the patients is uncontrolled. So we do not know whether the lungs of some patients responded better to the transplantation than other. We hope this information may become apparent in future studies.”
(ends)
Notes to editors
[1] Abstract no: 2 OA. “Autologous transplantation of P63+ lung progenitor cells for chronic obstructive pulmonary disease therapy”, by Prof. Wei Zuo et al. Presented in session “Innovative Approaches to Managing Asthma and COPD: A Translational Perspective” from 11.00-12.15 hrs CEST on Tuesday 12 September 2023. https://k4.ersnet.org/prod/v2/Front/Program/Session?e=379&session=16493
The research was accomplished in collaboration with Profs. Nanshan Zhong and Shiyue Li of the First Affiliated Hospital of Guangzhou Medical University, Guangzhou Institute of Respiratory Health, Guangzhou, China, and Prof. Xiaotian Dai, of Southwest Hospital, Third Medical University of PLA, Chongqing, China.
Funding: Regend Therapeutics Ltd, a Chinese biotech company, funded the clinical study.
The European Respiratory Society (ERS) International Congress is a once-a-year occasion when the world’s respiratory experts come together to present and discuss the latest research on topics such as asthma, COPD, lung cancer, pollution, smoking and COVID-19. The congress welcomes thousands of participants from all over the world each year, facilitating the exchange of scientific and clinical excellence across the entire field of respiratory medicine. The reputation of ERS derives from the outstanding scientific programme of its international congress, which this year is available to in person and online participants: www.ersnet.org/congress